Glaucoma
The term Glaucoma refers to a group of optic neuropathies which can result in progressive vision loss. It is the leading cause of irreversible blindness in the world. It has been estimated that 80 million people worldwide have glaucoma with 11.2 million bilaterally blind as a result.
Because age is a major risk factor and because life expectancies are increasing, the prevalence of glaucoma is also expected to increase in the coming decades.
Classically, glaucoma is correlated with the pressure within the eye. The intra ocular pressure (IOP) is a major risk factor in the development of glaucoma when elevated. However, it is not elevated in a substantial number of patients who still suffer from visual loss from glaucoma (normal tension glaucoma).
How Does The Pressure In The Eye Rise?
The eyeball is a closed system which makes its own fluid, called aqueous, to supply nutrients to its internal structures. In order for the eye to maintain a healthy pressure, it must also remove fluid or the pressure rises. If the pressure gets too high, the fibers which make up the optic nerve begin to die, thereby preventing the “picture” which is formed on the retina from reaching the brain – where we actually “see” an object.
Please consult the following video to better understand how the pressure rises in the eye.
Types Of Glaucoma
Adult forms of glaucoma are classified as Open Angle or Angle Closure Glaucoma.
OPEN ANGLE GLAUCOMA
Open angle glaucoma means that there is an elevated rise in the patient’s eye pressure without any apparent obstruction to the drainage area. In essence, the part of the patient’s eye that drains the internal fluid, called the trabecular meshwork (TM), does not seem to be functioning properly.
This is the most common type of glaucoma and the prevalence varies widely among samples of different ethnic and racial representation. The overall prevalence is 4-5 times higher among black individuals than white individuals.
The overall prevalence in North America is 3.3%.
The major risk factors for this type of glaucoma are: older age, high IOP, high myopia, thin corneas as well as ethnic, racial and genetic susceptibilities.
CLOSED ANGLE GLAUCOMA
In this type of glaucoma, there is partial or complete obstruction of the drainage system of the eye. The internal fluid of the eye can no longer drain out of the eye and the pressure therefore increases. In some cases the pressure can rise very fast , acute angle closure glaucoma or narrow angle glaucoma.
With angle closure glaucoma, the iris is not as wide and open as it should be. The outer edge of the iris bunches up over the drainage canals, when the pupil enlarges too much or too quickly. This can happen when entering a dark room.
A simple test can be used to see if your angle is normal and wide or abnormal and narrow. Treatment of angle closure glaucoma usually involves surgery to remove a small portion of the outer edge of the iris. This helps unblock the drainage canals so that the extra fluid can drain. Usually, surgery is successful and long lasting. However, you should still receive regular check-ups.
Symptoms of angle closure glaucoma may include headaches, eye pain, nausea, rainbows around lights at night, and very blurred vision.
Diagnosis & Treatment
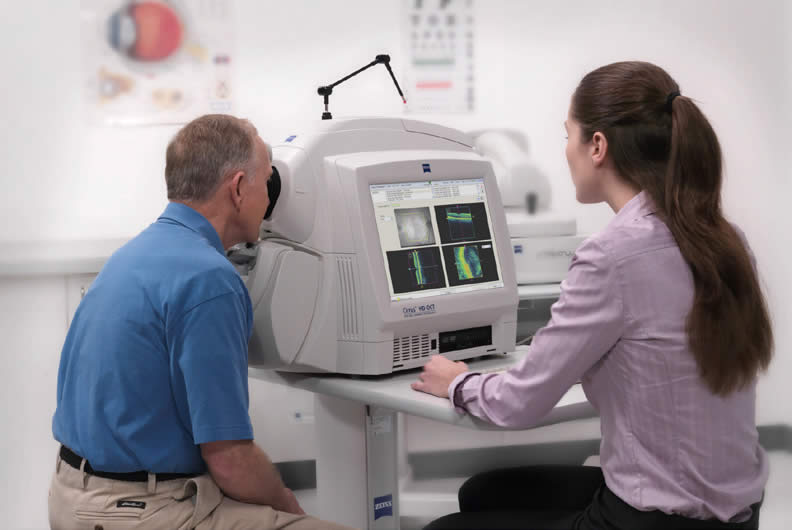
GLAUCOMA OCT
The key to preventing vision loss is early glaucoma detection. And, since your surgeon acquired the Optical Coherence Tomography, it has never been easier to be diagnosed for this blinding disease – often before vision suffers.
We have known for years the importance of the appearance of the optic nerve for the clinical assessment of glaucoma. This quantitative imaging device gives your doctor a way to obtain high resolution images that are both objective and reproducible. Also, the OCT has a normative database that can determine whether the measurements of your optic nerve are within the normal range or represent optic nerve damage.
The OCT exam is fast, safe, and usually does not require dilating the eye.
Gonioscopy
In order to diagnose your type of glaucoma, your doctor will perform a gonioscopy exam. This will help to determine whether you have open vs angle closure glaucoma.
This is a simple test performed with a local anesthetic drop that will allow your doctor to look into the eye and view the integrity of the drainage system with the use of a gonio lens.

VISUAL FIELD TESTING
The standard way to measure the visual field defects from glaucoma is a visual field test. This looks at the ability of the patient to detect a light stimulus on a uniformly illuminated background.
The test takes about 15 minutes. With regular visual field the doctor will be able to assess whether your glaucoma in well controlled or progressing.

Treatment of Glaucoma
OPEN ANGLE GLAUCOMA
Because there is no obvious blockage to the TM, your surgeon tries to decrease the amount of fluid the eye makes, or by artificially stimulating the TM to drain more fluid. In the United States, the most common initial measure to alter the internal production and/or drainage of aqueous is through the use of antiglaucoma medications. These medications are applied directly to the ocular surface in the form of drops. When medications fail to produce a desirable level of eye pressure control, the next level of treatment is typically a laser treatment called a trabeculoplasty.
SLT LASER
Laser trabeculoplasty is an office-based procedure where light energy is delivered to the drainage area of the eye and stimulates the TM to drain more fluid. Usually, the procedure takes only few minutes, is painless, and the patient is in a sitting position. It takes 4-6 weeks for the patient to experience a lowering of the eye pressure but the lowering affect could be seen up to six months after the procedure.
The SLT has allowed for an improved quality of life for thousands of patients around the world. In many countries including the US, SLT is used as a first line treatment, before glaucoma drugs. SLT patients do not need to take medications or at least as many medications. Studies have shown that less than 50% of glaucoma patients actually take their medications as prescribed and many stop taking them due to the numerous side effects experienced, cost, busy lifestyle and all other daily variables and challenges we all experience. Compliance is now controlled by your physician. The low percentage of non-responders to SLT therapy can simply begin traditional medications.

The benefits of SLT Therapy are:
- Improve your quality of life
- Eliminate or reduce your immediate need for medications
- Allows the eye to naturally heal itself
- Can be repeated if necessary
- No systemic side effects
Due to the nondestructive nature of SLT Therapy unlike traditional laser therapy, SLT can be used for the following conditions:
- Primary Open Angle Glaucoma
- Ocular Hypertension
- Normal Tension Glaucoma
- Juvenile Glaucoma
- Aphakic Glaucoma
- Pigmentary Glaucoma
Acute Angle closure glaucoma or Narrow Angle glaucoma
Acute angle closure glaucoma is a medical emergency. There is an acute blockage of the drainage system of the eye and the pressure can rise very fast. This type of glaucoma is not as prevalent as the open angle glaucoma. The patient typically presents with pain, headache, blurred vision and halos around lights.
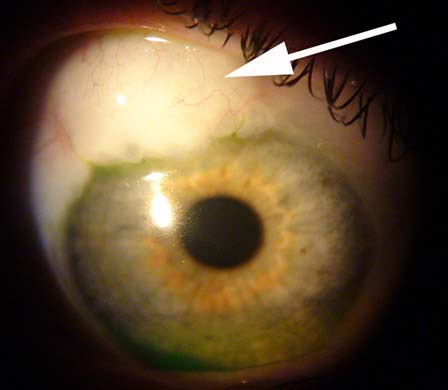
The definitive treatment for this condition is a laser procedure called Peripheral iridotomy where the surgeon uses a laser to relieve the blockage of the drainage system of the eye. This is an in-office procedure.
When all other treatment measures fail, the next step is surgical control of intraocular pressure. The reasoning is, if medical and laser therapy are not capable of stimulating the TM to drain enough aqueous to keep the eye pressure low, then a new route of egress for the fluid needs to be made in order to lower the patient’s eye pressure to an appropriate level.
MIGS or Minimally Invasive Glaucoma Surgeries
Being fellowship trained in glaucoma, Dr. Rioux is proud to offer you some of the most advanced glaucoma surgeries and procedures which have revolutionized the paradox in glaucoma treatment in the past decade.
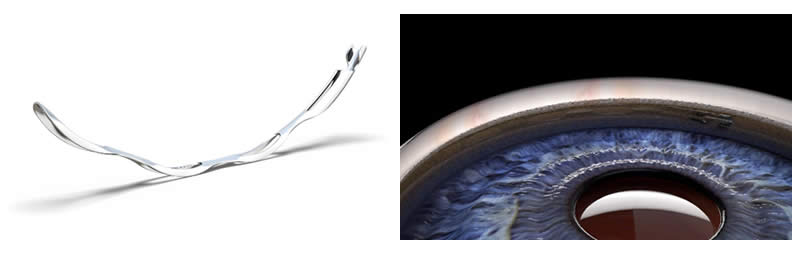
The Hydrus microstent by Ivantis
The Hydrus Microstent is an innovative MIGS devise designed to relieve the intra ocular pressure in the eye. It is roughly the size of an eyelash and it reduces the eye pressure by reestablishing the patient’s natural outflow pathway through which fluid exits the eye. It is placed in the eye by a surgeon using a small incision in a minimally invasive procedure. This less invasive approach may allow for fewer complications and faster recovery than traditional incisional glaucoma surgeries.

OMNI PROCEDURE BY SIGHT SCIENCE
The Omni is a MIGS procedure where your surgeon dilates the drainage of the eye (canaloplasty) and alleviates the resistance (goniotomy) to allow better flow of the fluid in the eye, out of the eye.
Conventional Glaucoma Procedures:
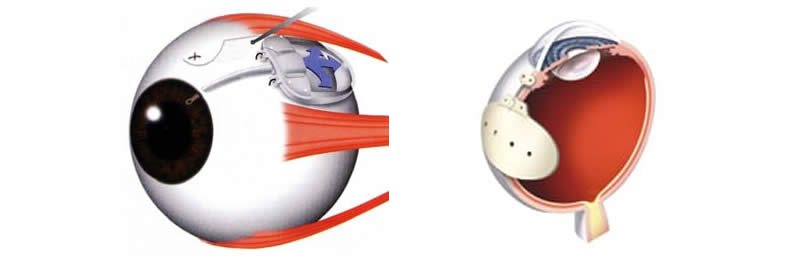
Trabeculectomy and tube shunts
For patients who are not good candidates for MIGS ,either because their glaucoma is too advanced or if one can not visualize the angle for angle surgeries(MIGS), a trabeculectomy or a valve surgery is therefore required.
Trabeculectomy
A trabeculectomy is an incisional procedure which allows the intraocular fluid to drain out of the eye by bypassing the normal pathway.
It is indicated when maximum tolerated medical treatment and lasers fail to stop the progression of glaucoma.
It is performed in the operated room under sedation. The patient goes home the same day with a patch over the eye.
Tube shunts
There are a number of tube shunts your surgeon can choose from (Ahmed,Baerveldt, Molteno).
The shunt will allow the intraocular fluid to shunt to a plate in the subconjunctival space out of the eye.
The indications are the same as the trabeculectomy: failed medical or surgical treatment to stabilize the glaucoma. It may be the best choice for eyes with excessive scar tissue (eg: failed prior trabeculectomy).